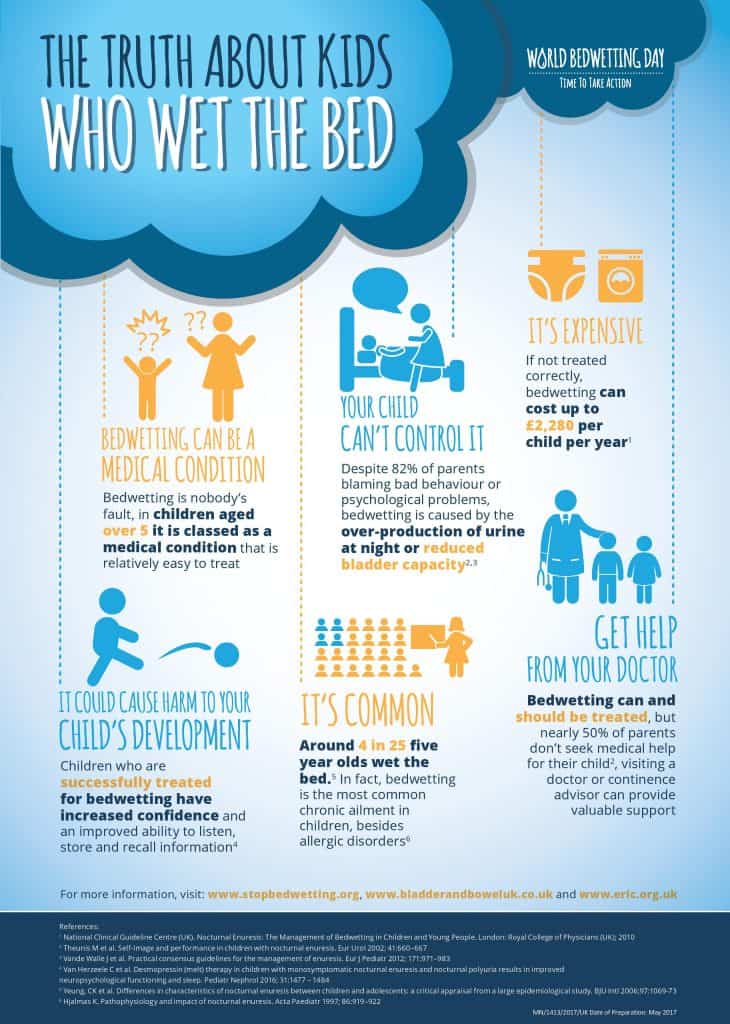
On World Bedwetting Day, new global guidelines call for more effective treatment for the 4 in 25 children living with this common medical condition 1
- Bedwetting is a common problem affecting 16% of five-year olds 1
- There are suggestions of a genetic link in bedwetting, with a risk of 44% if one parent used to wet the bed and 77% if they both did 2
- Bedwetting has a serious impact on a child’s self-esteem, emotional well-being, daytime functioning and school performance 3,4,5
- Treatment is available, yet in most cases there is almost a 3-year delay before a child is seen by a healthcare professional 6
West Drayton, England, UK – 30th May, 2017 – Today is World Bedwetting Day and this year’s theme is ‘Time to Take Action’, raising awareness that children don’t need to suffer with bedwetting, and that more can be done to diagnose and treat children who struggle with this condition.
Bedwetting is nobody’s fault, and families and doctors should be able to discuss the condition without embarrassment or guilt. However, the impact of this condition is often underestimated and trivialised, so help is usually not sought or offered.7 By raising awareness of bedwetting as a common condition that can and should be treated,8 World Bedwetting Day aims to encourage families to discuss bedwetting with their doctors and get children the help they need.
To coincide with World Bedwetting Day, the World Bedwetting Day Steering Committee (WBD-SC) has launched simplified practical guidelines to help healthcare professionals (HCPs) understand how to best treat bedwetting. “For decades, people thought children would simply outgrow wetting the bed, but we now know that it is a common medical condition which can be treated relatively easily,” says June Rogers MBE, Paediatric Continence Specialist, Bladder and Bowel UK. “This new guidance ensures all HCPs have clear information on how to manage bedwetting; the next challenge is to make sure the parents of children who struggle with bedwetting know they can speak to their doctor or nurse and that help is available.”
Bedwetting is a common medical condition affecting around 4 in 25 five year old children.1 For decades, it has been considered a simple condition that would resolve spontaneously. However, it is now regarded as a complex disorder involving several factors, such as bladder dysfunction and the over-production of urine at night.3
The condition can have a serious impact on a child’s self-esteem, emotional well-being and daily activities, including school performance and social interactions.2,3,5 Children who have been successfully treated for bedwetting have shown an improved auditory memory – the brain function required for listening, storing and recalling information.9 Although bedwetting causes a significant impact on children and their families, training for HCPs rarely includes specific guidance on bedwetting and how it should be addressed. Using the worldwide input of the WBD-SC members, the newly released guidelines act as a clear, reliable source of information for HCPs across the globe to improve the journey to diagnosis and treatment, ultimately reducing the impact of bedwetting on families.
Brenda Cheer, Paediatric Specialist Continence Nurse and the ERIC Nurse said: “This year’s World Bedwetting Day message that this common childhood condition can and should be treated is one that we echo at ERIC. Left untreated, bedwetting won’t necessarily go away on its own and not all children ‘get dry in their own time’. Dealing with bedwetting can have a serious impact on a child’s well being and selfesteem. Half of parents whose children wet the bed don’t seek medical advice. We want all parents and carers of children and teenagers who are wet at night not to delay but to seek the help that is out there.”
For more information, visit: www.stopbedwetting.org, www.bladderandboweluk.co.uk and www.eric.org.uk